Progression from symptom onset to the diagnosis of spasmodic dysphonia
People with spasmodic dysphonia initially notice either a gradual or sudden onset of difficulty in speaking. They may hear breaks in their voice during production of certain words or speech sounds, breathy-sounding pauses on certain words or sounds, or a tremulous shaking of the voice. They may feel that talking requires more effort than before. Often people say that their voice sounds as if they “have a cold or laryngitis.”
The symptoms of SD can vary from mild to severe. A person’s voice can sound strained, tight, strangled, breathy, or whispery. The spasms often interrupt the sound, squeezing the voice to nothing or dropping it to a whisper. Just like with any health issue, stress can worsen the symptoms, but it is not the cause of them.
Onset is usually gradual with no obvious explanation. Symptoms occur in the absence of any structural abnormality of the larynx, such as nodules, polyps, carcinogens, or inflammation. People have described their symptoms as worsening over an approximate 18-month period and then remaining stable in severity from that point onward. Some people have reported brief periods of remission, however this is very rare and the symptoms usually return.
Getting a proper diagnosis-where to start
Spasmodic dysphonia can be difficult to diagnose because the anatomy of the larynx is normal. SD has no objective pathology that is evident through x-rays or imaging studies like a CT or MRI scan, nor can a blood test reveal any particular fault. In addition, several other voice disorders may mimic or sound similar to it.
The excessive strain and misuse of muscle tension dysphonia (MTD), the harsh strained voice of certain neurological conditions, the weak voice symptoms of Parkinson’s disease, certain psychogenic voice problems, acid reflux, or voice tremor are often confused with SD. Therefore, the best way to diagnose the problem is to find an experienced clinician with a good ear.
Getting a diagnosis can be a team effort. This is why it is important to prepare before you visit your physician and be prepared to communicate effectively. Don’t hesitate to ask any questions needed in order to fully understand your diagnosis. This applies to dealing with your initial diagnosis, the frustrations of treating your SD, and how to effectively cope.
Visiting Your Primary Care Doctor
Your visit with your primary care doctor may be frustrating. There are so many causes of vocal issues that it may require the approach of ruling out other things before settling on the correct diagnosis or being sent to a specialist.
Take a list of questions to your doctor — When you are dealing with this new diagnosis it is easy to become overwhelmed and forget what you wanted to ask. Writing out your list can help. Start by prioritizing your questions and ask the questions that are most important to you first. As you ask questions and think of additional questions, jot down the new ones at the bottom of your list. Questions to ask:
1. What do you think is causing my problem?
2. What is my diagnosis?
3. Is there more than one condition that could be causing or contributing to my problem?
4. Since there are so many causes for voice issues, how certain are you with regard to this diagnosis.
5. Do I need to seek input from any other medical professionals like and ENT?
If you are referred to an ENT, it would be best to seek out one that has experience with voice issues.
Visiting an Otolaryngologist (ENT)
Seek out an Ear Nose and Throat (ENT) doctor, or otolaryngologist, that has experience with voice issues or specializes in voice issues. You may be referred to a subspecialist called a laryngologist. Laryngology is a subspecialty within otolaryngology (ear, nose, and throat) that deals with disorders of voice, airway and swallowing. Through postgraduate fellowship training, a laryngologist has special expertise in the diagnostic and therapeutic approaches to problems in these areas. This way you have a physician focused on the voice who can help get your voice issue diagnosed quickly. Check out our healthcare referral list to find someone who specializes in voice disorders.
Suggested List of Questions:
1. What test will you do to diagnose the problem? How accurate is the test at diagnosing my problem? Are there other diagnostic tools available that would confirm the diagnosis?
2. Upon diagnosis, ask what is the likely course of this condition?
3. What is the most conservative approach to try first? What happens if this treatment does not work?
4. Will treatment affect the long-term outlook?
5. How will I know when I have reached my plateau?
6. What changes will I need to make?
7. What organizations/resources are available to help me with making these changes?
8. Where can I find information about clinical trials/research being conducted on SD?
9. Is there a chance that anyone else in my family may get this condition?
10. What tools are available that will help me with the tasks that are difficult for me (voice amplifiers, telephones)?
11. Are my symptoms “normal?” What if I have atypical symptoms? Do I know when a symptom is not SD?
12. Long-term outlook: Does SD progress in severity? Will it go into remission? Will treatments affect the progression?
Take a companion with you to take notes– — Bringing someone for support will allow you to focus on asking the questions and understanding the answers without the pressure of having to remember every detail. Afterwards you can review the information to make sure your understanding matches that of your companion. You can also ask your doctor to send you a copy of your evaluation results and the recommended treatment options for you to review.
Visiting an Speech-Language Pathologist (SLP)
A Speech-Language Pathologist (SLP) can help manage symptoms and is often used in conjunction with an ENT to confirm diagnosis. They will:
1. Work with spasms/tremor, not suppress them
2. Improve the ease and quality of voice production
3. Increase the awareness and ability to manage vocal variations
An SLP will create an individualized plan, and work on techniques such as breathing control, which involves maintaining a steady flow of air from the lungs during voice production, relaxation, and pitch and loudness modifications can help improve the person’s voice.
Questions to ask:
1. What can I expect from voice therapy?
2. How long should we try this before quitting?
3. Why do I need voice therapy?
4. How many SD patients have you worked with?
5. If voice therapy is working, does that mean I do not have SD?
6. Will I be able to sing (or whatever you are concerned about) again?
7. Should I use voice amplification devices?
In addition, voice therapy should be considered when a person has Muscle Tension Dysphonia (MTD) along with SD.
Click here to find an SLP in our Healthcare Referral Database
Visiting a Neurologist
Since some voice disorders like SD have a neurological component, an appointment with a neurologist that focuses on movement disorders, will help determine if there is a neurological component present.
What to expect during the exam
After taking the medical history, your medical professional will listen carefully to your speech to identify specific signs of SD, such as voice breaks. To help differentiate the condition and sub-type, they often ask the patient to read and speak specific phrases and sentences loaded with certain types of sounds. While additional evaluations may help to determine the diagnosis, often times, the experienced clinician expert’s perceptual analysis usually serves as the basis for making the SD diagnosis.
The physical examination continues by looking at the larynx in action. Even though the person with SD often has a normal anatomy, the physician should look at the larynx to rule out other common laryngeal disorders that can result in a hoarse voice. These include a wide variety of conditions that range from benign issues such as vocal cord nodules or polyps, to more concerning conditions such as vocal cord cancer.
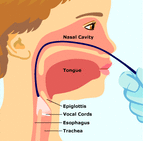
One way to view the larynx is to insert a rigid endoscope, a straight, narrow metal rod containing a variety of lenses, through the mouth and toward the back of the throat while the person is saying “eeeee.” In this manner, the otolaryngologist obtains a close-up view of the structures of the larynx and the movement of the vocal folds.
Another common approach to viewing the vocal folds involves the use of a flexible endoscope. In this method, a very narrow, flexible tube with a lens is inserted through one nostril, around the back of the nose and down through the throat. This allows the doctor to evaluate the movements of the larynx while the person is speaking or singing.
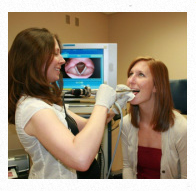
Usually these endoscopic examinations are performed with a specialized flickering light called a “stroboscope,” which allows the clinician to further evaluate the rapid fine movement of the vocal folds. These evaluations can be recorded for both the clinician and patient to review after the examination.
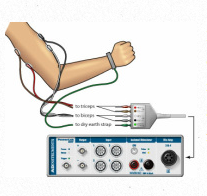
In addition to these tests, the otolaryngologist may recommend a laryngeal electromyography (EMG) test to obtain specific information about the specific muscles involved. The EMG test involves inserting a thin needle electrode through the neck into the muscles of the larynx and evaluating the electrical activity of the muscles at rest and during speaking. While some fine the EMG helpful, there are no specific types of signals that are diagnostic of only SD. With a confirmed diagnosis, the doctor can work with you to find the best course of treatment for your symptoms.
Once a diagnosis of SD is made, you should continue to take an active role in your health care. Ask questions, record the answers, get second opinions when necessary, and become fully educated about the condition and the treatment options.
Spasmodic dysphonia is estimated to affect approximately 50,000 people in North America, but this number may be inaccurate due to ongoing misdiagnosis or undiagnosed cases of the disorder. Although it can start at any time during life, SD seems to begin more often when people are middle-aged. The disorder affects women more often than men.
Image source: https://spasmodicdysphoniawku.weebly.com/evaluation.html


