Type II Thyroplasty: A Surgical Treatment for Adductor Spasmodic Dysphonia
Type II Thyroplasty is a surgical procedure that separates the vocal folds and it is used to treat the adductor form of spasmodic dysphonia. It is reasoned that speaking in those with AdSD is affected due to the tight closure of the vocal folds during speech. During the procedure, the surgeon physically separates the vocal folds to limit their ability to excessively contact one another. A titanium bridge is inserted to maintain the separation. The operation is typically performed under local anesthesia with sedation so that the patient can talk while the surgeon adjusts the vocal folds to the optimal distance. The result is a slightly weaker and breathier voice with improved fluency. Long term outcomes have not yet been published.
This procedure was developed by Dr. Isshiki and his group around 2000. The concept of this surgery is aiming to smooth the airflow by making the glottal gap wider during phonation. The titanium bridges used in this procedure are manufactured and approved for use in Japan only at the Isshiki Memorial Voice Center. They are not FDA approved and not yet available for use in the United States. The NSDA has been working with Nobel Pharma to bring these bridges to the US for a clinical trial for adductor spasmodic dysphonia.
Benefits of Type II Thyroplasty
– Effect is stable and vocal improvement is sustained
– Intraoperative adjustment is possible
– No direct surgical intervention into the vocal folds, reducing the risk of scarring
– There is no disability created (such as paralysis)
– Procedure is reversible
– Rare but possible postoperative hemorrhage
Best Candidates for Type II Thyroplasty
— Those with adductor spasmodic dysphonia
— Those who obtain good results from botulinum neurotoxin treatment
Poor Candidates for Type II Thyroplasty
— Those with abductor form of spasmodic dysphonia
— Those with adductor spasmodic dysphonia combined with a tremor
— Those with adductor spasmodic dysphonia who do not respond to botulinum neurotoxin injections
Information about the Procedure
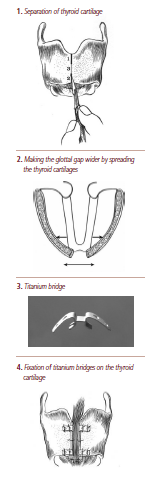
Following local anesthesia using xylocaine, 4 cm (1.5 inches) of horizontal skin incision is made at the front of neck to expose the laryngeal cartilage.
Thyroid cartilage is carefully separated at the midline to avoid perforating the larynx lumen. By spreading both sides of the thyroid cartilage, the anterior glottal gap becomes wider, and then the airflow through the vocal folds becomes smooth and the voice strangulation is relieved.
The gap between both sides of the thyroid cartilage can be adjusted so that patients are asked to speak during the procedure to find the most appropriate gap which makes patients feel there is least strangulation.
After determining this gap, the corresponding size titanium bridges (2.0 to 5.0 mm) which were specially made for this surgery are placed and fixed by nylon suture at the superior and inferior part of the gap between both sides of the thyroid cartilages. Surgery is finished by closing the skin incision.
The procedure lasts for one to two hours. Patients are allowed to speak three days after the surgery, and can talk loudly one month afterwards. A possible complication which could be serious is postoperative hemorrhage resulting in airway obstruction, however, this has never been experienced.
Recovery time and risks are minimal, making this operation a reasonable option despite the variability of results. Most patients experienced improvement in vocal quality, however, recurrence of symptoms has been noted between 3-5 years.
Reported Results
Reported results from Isshiki Memorial Voice Center of over 500 AdSD patients in the last 5 years:
— 60% were very satisfied with the results
— 30% were reasonably satisfied with the results
— 10% were unsatisfied with the results due to breathy voice quality
— 1% required removal of the titanium bridge due severe breathy voice
The team reports they have never experienced dislocation of titanium bridges, but a small number of fractures were detected by regular CT scan several years after surgery. Even when titanium bridges were fractured, the voice never went back to the preoperative status since scar formation surrounding the titanium bridges altered the role of titanium bridges.


